2020
HRSA Responds to the COVID-19 Pandemic While Celebrating 30 Years of RWHAP
In 2020, the Health Resources and Services Administration (HRSA) celebrated the 30-year anniversary of the historic legislation that created the Ryan White HIV/AIDS Program (RWHAP), commemorating three decades of providing HIV primary medical care, essential support services, and medications for low-income people with HIV. Signed into law on August 18, 1990, the Ryan White Comprehensive AIDS Resources Emergency (CARE) Act created the largest federal program focused uniquely on HIV care and treatment, which today provides services to more than half-a-million people each year.
Thirty years later, the RWHAP continues its commitment to addressing health disparities in underserved communities and ensuring access to and retention in high-quality, integrated care and treatment services for all people with HIV as RWHAP continues to move forward with ending the HIV epidemic in the United States. Since 2020, the RWHAP has had a critical role in the Ending the HIV Epidemic (EHE) initiative, which aims to reduce new HIV infections in the United States by 90 percent by 2030.
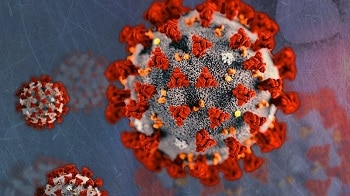
COVID-19 and Its Effects
Despite the promising scientific and programmatic advancements in HIV care and treatment, however, 2020 was characterized by a different viral disease: coronavirus disease 2019, or COVID-19. When the COVID 19 public health emergency first began in early 2020, it presented an immense challenge to delivering HIV care and services to people with HIV. COVID-19-induced quarantines and social distancing measures changed the way in which RWHAP patients, clients, and their family members were able to access critical health care services and basic care needs, such as access to medication, transportation, and food services.
Despite its challenges, the COVID-19 public health emergency gave RWHAP providers the opportunity to think innovatively and implement new approaches to HIV care and client engagement.
Use of Telehealth
The use of telehealth among RWHAP providers and clients was widely adopted during the pandemic as a result of additional funding. Although some RWHAP providers had already implemented telehealth to assist people with HIV seeking care, the technology was applied more widely during the pandemic. Based on preliminary data from the November 2020 COVID-19 Data Report, approximately 84 percent of RWHAP providers consistently reported having increased telehealth capacity, up from 69 percent in March 2020. Telehealth not only ensured continuity of care but, in some cases, improved care and client engagement.
Benefits of Telehealth
- RWHAP providers have reported more frequent and longer meetings between staff and patients, with a lower rate of missed appointments among patients.
- Being able to see patients’ homes enabled providers to evaluate patients’ living conditions, diets, and lifestyles directly, which helped them address the specific needs of their patients.
- Telehealth also has enabled providers to conduct psychosocial and mental health care assessments, services that are particularly critical for patients coping with the trauma and isolation of a pandemic.
Further Flexibility in Services
Beyond implementing telehealth, RWHAP providers also have offered adapted services that have helped patients avoid travel. Such adaptations include home-based self-testing for sexually transmitted infections and HIV, virtual signatures, medical home-delivery services, and extended prescriptions. For example, a medication that normally would be filled for 30 days would be filled for 90 days, thereby preventing the need for patients to make monthly trips to the pharmacy. Other providers re-evaluated certification and recertification processes to make them more flexible.
Although 2020 was a challenging year, the RWHAP played an integral role in the COVID-19 response while continuing to support its EHE goals. Undaunted, the RWHAP saw the COVID 19 pandemic not as a roadblock, but as a means of paving the way for change. RWHAP providers ensured continuity of care for people with HIV and their families during the pandemic through innovative care delivery and engagement methods. The unique needs of people with HIV were addressed during a time in which health was paramount, and the adaptive changes made during this time are ones that likely will continue into 2021 and beyond.
 Health Resources & Services Administration
Health Resources & Services Administration